January 13, 2026
By: Brionna Benedetti, Manager of Value-Based Coding
2025 Financial Impact
As we close out the 2025 calendar year, we as a network can now begin to reflect on all lessons learned and plan for a successful 2026. One challenge that the network collectively faced in 2025 was the spend associated with treating chronic kidney disease (CKD) for the attributed patient population.
In 2025, there were over 900 patients with CKD within the straight Medicare population alone. This population of Medicare patients, while seemingly small when divided by CHC attribution, accounted for over $7,000,000 worth of claims for their care.
Kidney disease is a costly condition to treat, so what can we do as a network to reasonably reduce the spend utilization for this population? The answer is not reducing the patients’ care, or limiting their access to treatment, but rather ensuring that we are consistently reporting and appropriately staging the patients’ CKD to the payers, through claims.
| Stage of CKD | Carina Network CKD Spend (claims data as of 1/9/2026) | 2025 Lost Benchmark Spend |
| Stage 1 | $2,206.31 | |
| Stage 2 (mild) | $267,039.40 | |
| Stage 3 unspecified | $577,967.43 | $69,175.63 |
| Stage 3a | $1,346,470.21 | $110,691.45 |
| Stage 3b | $1,520,651.58 | $40,454.75 |
| Stage 4 (severe) | $962,407.52 | $140,650.00 |
| Stage 5 | $70,095.28 | |
| End stage renal disease (ESRD) | $2,564,064.46 | $19,878.87 |
| Grand Total | $7,310,902.19 | $380,850.70 |
2025 Coding Trends
In 2025, 21% of the CKD conditions previously recaptured for patients in past years were not recaptured in claims, leaving over $380,000 in benchmark budget unaccounted for. While patients with CKD may spend more than that based on their claims data, the appropriate coding of a patient’s CKD is a vital first step to ensuring that needed funding is provided for the patients to account for their healthcare needs.
Documentation
CKD is a long-standing, progressive deterioration of renal function and should be recaptured yearly via claims. To capture CKD appropriately, documentation in the encounter note is needed to describe:
- CKD Stage,
- Cause of CKD (if CKD is secondary),
- Current status of CKD (stable, worsening, improved, etc.),
- Comorbidities and complications (if present),
- Current disease management,
- and current treatment plans.
| CKD Stage | ICD-10 Code | GFR Range |
| Stage 1 | N18.1 | >90 mL/min |
| Stage 2 | N18.2 | 60-89 mL/min |
| Stage 3, Unspecified | N18.30 | 30-59 mL/min |
| Stage 3a | N18.31 | 45-59 mL/min |
| Stage 3b | N18.32 | 30-44 mL/min |
| Stage 4 | N18.4 | 15-29 mL/min |
| Stage 5 | N18.5 | <15 mL/min |
| End Stage Renal Disease (ESRD) | N18.6 | <15 mL/min (with dialysis) |
Unspecified CKD (N18.9) should not be documented if the stage of CKD is known and more specific. The stage of CKD cannot be determined by a coder based on GFR values alone. It is important that the provider notes the CKD stage when known, as a coder does not have the authority to assign or alter a code selected without the providers express documentation, with a few exceptions we will discuss later in the guide. If a provider documents both CKD and ESRD, the coder should only code for ESRD.
Do not document “history of” to describe current chronic kidney disease. In diagnosis coding, the phrase “history of” means the condition is historical and no longer exists as a current problem. A provider should also avoid documenting CKD as current when the condition is truly historical and no longer exists as a current problem. This can be tricky for patients who have a history of CKD that resolved due to a kidney transplant.
Warning: Per ICD-10 Guideline I.C.14.a.2, a patient can still have some form of CKD after a kidney transplant, as the transplant may not restore all kidney function. The presence of CKD after transplant does not automatically indicate a transplant complication. If a coder is unsure if CKD is present after a transplant has taken place, query the provider.
Coding
Renal insufficiency (N28.9) is a general term that should be avoided when a specific CKD stage is documented. Use the most specific code possible. Coding for CKD can depend on the complications and manifestations of the CKD at the moment of the encounter:
Acute on Chronic CKD
If a patient presents with both acute kidney failure (N17.-) and chronic CKD (N18.-), code both the acute and chronic CKD, with acute CKD being sequenced first.
Hypertension with CKD
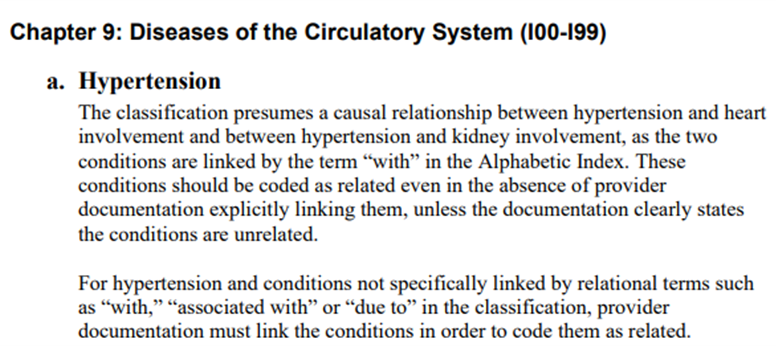
Per ICD-10-CM coding guideline I.C.9.a, there is an assumed causal correlation between hypertension and CKD. Comorbidities that are linked to hypertension in the ICD-10-CM using the term “with”. Comorbidities found under the “with” below the code title should be interpreted to mean “associated with” or “due to.”
This classification presumes a causal relationship between the two conditions even in the absence of provider documentation explicitly linking them. This means coders can code to higher specificity even when not directly correlated in providers’ documentation when a comorbidity is present. However, if the documentation clearly states that the two conditions are not related, then the combination code should not be selected.
If a patient has hypertensive CKD and acute renal failure, the acute renal failure should also be coded, but sequencing can depend on the circumstances of the encounter.
| ICD-10 Code | Code Description | Code Also |
| I12.0 | Hypertensive chronic kidney disease with stage 5 chronic kidney disease or end stage renal disease | Use additional code to identify the stage of chronic kidney disease (N18.5, N18.6). |
| I12.9 | Hypertensive chronic kidney disease with stage 1 through stage 4 chronic kidney disease, or unspecified chronic kidney disease | Use additional code to identify the stage of chronic kidney disease (N18.1-N18.4, N18.9). |
| I13.0 | Hypertensive heart and chronic kidney disease with heart failure and stage 1 through stage 4 chronic kidney disease, or unspecified chronic kidney disease | Use additional code to identify type of heart failure (I50.-) and stage of chronic kidney disease (N18.1-N18.4, N18.9). |
| I13.10 | Hypertensive heart and chronic kidney disease without heart failure, with stage 1 through stage 4 chronic kidney disease, or unspecified chronic kidney disease | Use additional code to identify the stage of chronic kidney disease (N18.5, N18.6). |
| I13.11 | Hypertensive heart and chronic kidney disease without heart failure, with stage 5 chronic kidney disease, or end stage renal disease | Use additional code to identify the stage of chronic kidney disease (N18.5, N18.6). |
| I13.2 | Hypertensive heart and chronic kidney disease with heart failure and with stage 5 chronic kidney disease, or end stage renal disease | Use additional code to identify type of heart failure (I50.-) and he stage of chronic kidney disease (N18.5, N18.6) |
| Secondary Hypertension | ||
| I15.1 | Hypertension secondary to other renal disorders | Code also underlying condition causing the hypertension. |
Diabetes with CKD
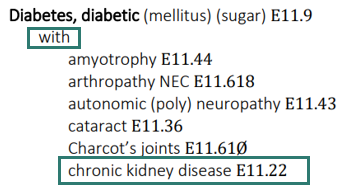
Diabetes mellitus is coded from categories E08 – E13, with additional characters following the base category code. These additional characters are used to detail the comorbidities and complications associated with diabetes when present. Per the ICD-10-CM guideline section I.A.15 the term “with” presumes cause-and-effect linkage between diabetes and certain conditions that appear in the alphabetic index as indented sub terms under the types of Diabetes. Unless the physician specifically indicates that the conditions are not related, these combination codes can be assigned even in the absence of provider documentation explicitly linking them. CKD is a comorbidity listed under the term “with”, meaning a combination code should be used when the comorbidity is present.
| Comorbidities and Complications | Secondary Diabetes | Drug or Chemical Induced | Type I | Type II | Other Diabetes |
| Diabetes with CKD *Add code for CKD Stage (N18.1-N18.9) and Z99.2 if on dialysis | E08.22 | E09.22 | E10.22 | E11.22 | E13.22 |
Use Additional Codes
It can be just as important to document and apply status codes that relay the types of treatment the patient is undertaking, as these treatments can be costly and add complexity to the patient’s care.
- Kidney transplant status (Z94.0)
- Dialysis status (Z99.2)
References
- ICD-10-CM
- ADA-Know-the-Stages.pdf
Download the full guide: Chronic Kidney Disease Coding Guide (plus more at https://carinahealthnetwork.org/guides-tools/)